Thud, crack, smack
Thud.. crack.. smack..
I don’t remember how it felt. I don’t even remember if that’s the exact sound it made. But I can be certain that’s how you’d describe my head impacting the ground.
Forehead, cheek, eye & chin - I did a good job of messing myself up. Lots of blood.
Just a few minutes before I was having a chat with my mate Ryan. We debriefed each other on how we’d had a sweet Christmas & New Year break and were both getting re-set to start the work year the next coming Monday. 2020 was here – it was going to be even more full on than usual, shaping up to be a year of promise as not only did I have a few personal & work goals planned to achieve, but my partner & I also had twin babies on the way.
After our catch up, we picked up our bikes & headed off down one of the trails. Ryan headed off first. We were both pretty capable & experienced riders but we didn’t pick a gnarly track - it was just a chance for a ride & to enjoy the great outdoors. He told me how at one point he stopped & turned around to ask me something, but I wasn’t there. He waited a minute and then got a bit worried as it wasn’t like me to be far behind him. He waited a minute or so more, then had a funny feeling so walked back up the track to find me lying on the ground; barely conscious, covered in blood and my arm snapped with broken bones protruding out from the skin.
It must have been a sight he walked into, but thank god he’s a great mate who acted so calmly & swiftly to let the emergency crew know there’d been a nasty accident, ensured they knew where I was & were able to get to the scene to give first aid to stabilise me, then get me via a stretcher on the back of an ATV to a sealed road so the ambulance could pick me up. I can’t even remember that happening or being transported to the Hospital A&E.
I was told I was assessed pretty quickly by the A&E staff who had me on some wonder painkillers, rushed me into the operating theatre to sort my arm & then passed me into the care of the ICU ward under the care of the Neurology team. I spent the next 6 days in that ward on morphine, oxygen and generally looking & feeling like I’d had 10 rounds in a boxing ring. Still none of it I remember. Nothing.
It was the post-traumatic amnesia that meant the first real memory of my hospital stay was looking up & seeing the curtain around my bed. From that point I can remember so many feelings I had; fatigue - I was pretty tired and fatigue came on quickly; confused - what had happened & why was I here; in pain – why am I half broken; frustrated - I just wasn’t the usual ‘me’. Normally being active & having so much on the go at once it was obviously a shock to the system as I was confined to my bed initially, then had a struggle just to walk (call that shuffle) a few metres around the ward.
I had some great visits from my family & my work colleagues but it I’ve heard it wasn’t all fun times for them as I was a bit vague, often jumbled and my memory was shot. I kept forgetting & repeating myself over & over, “Why don’t I have a TV in my room?”. 2 minutes later, “Why don’t I have a TV in my room?”.
As the days went on, I got a fraction better. I could eat my own dinner (no more spoon feeding!) & could even manage a trip to the bathroom or shower by myself. So a fraction better, but still a long, long way from right.
My rehab journey
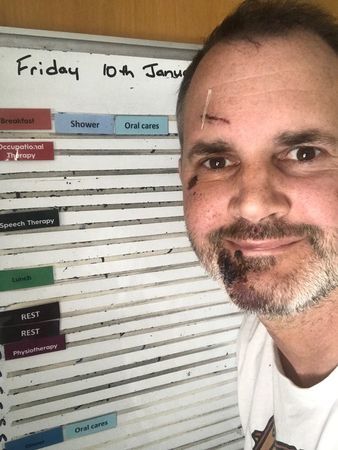
One day I was told I was being transferred from my hospital ward to a Rehabilitation Unit run by the Laura Fergusson Trust in Burnside. News to me who the organisation was, but my family told me it was a positive step to be leaving the Neurology Ward & heading to the Traumatic Brain Injury Unit. It was over my head so I just went with what I was told. The taxi ride seemed wondrous to me & took it out of me, but I arrived at a comfy & secure facility where I would have my own room, a schedule to help me slowly remember the patterns of daily life, 3 meals a day and a great team of support staff to help me – Psychologists, Doctors, Speech & Language Therapists, Physios, Occupational Therapist & I can’t forget the lovely Nurses.
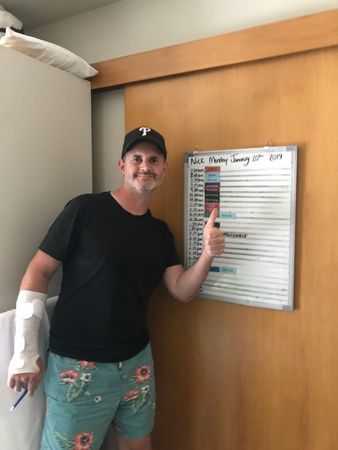
I got to know everyone during the next 2 week stay as I was one of the only patients in the unit for the majority of my time. It was all foreign to me but the staff were friendly, supportive & were always patient – the place felt more welcoming than where I’d come from. I had a TV to watch at last, nice people to chat to & always had a person to help keep me on schedule & remind me what was coming up next.
I had my wounds dressed, help with my medications & a multitude of assessments done on how I was – my fatigue levels, my memory, cognitive thinking skills, processing information, speech, writing, my emotions, what did I find challenging.
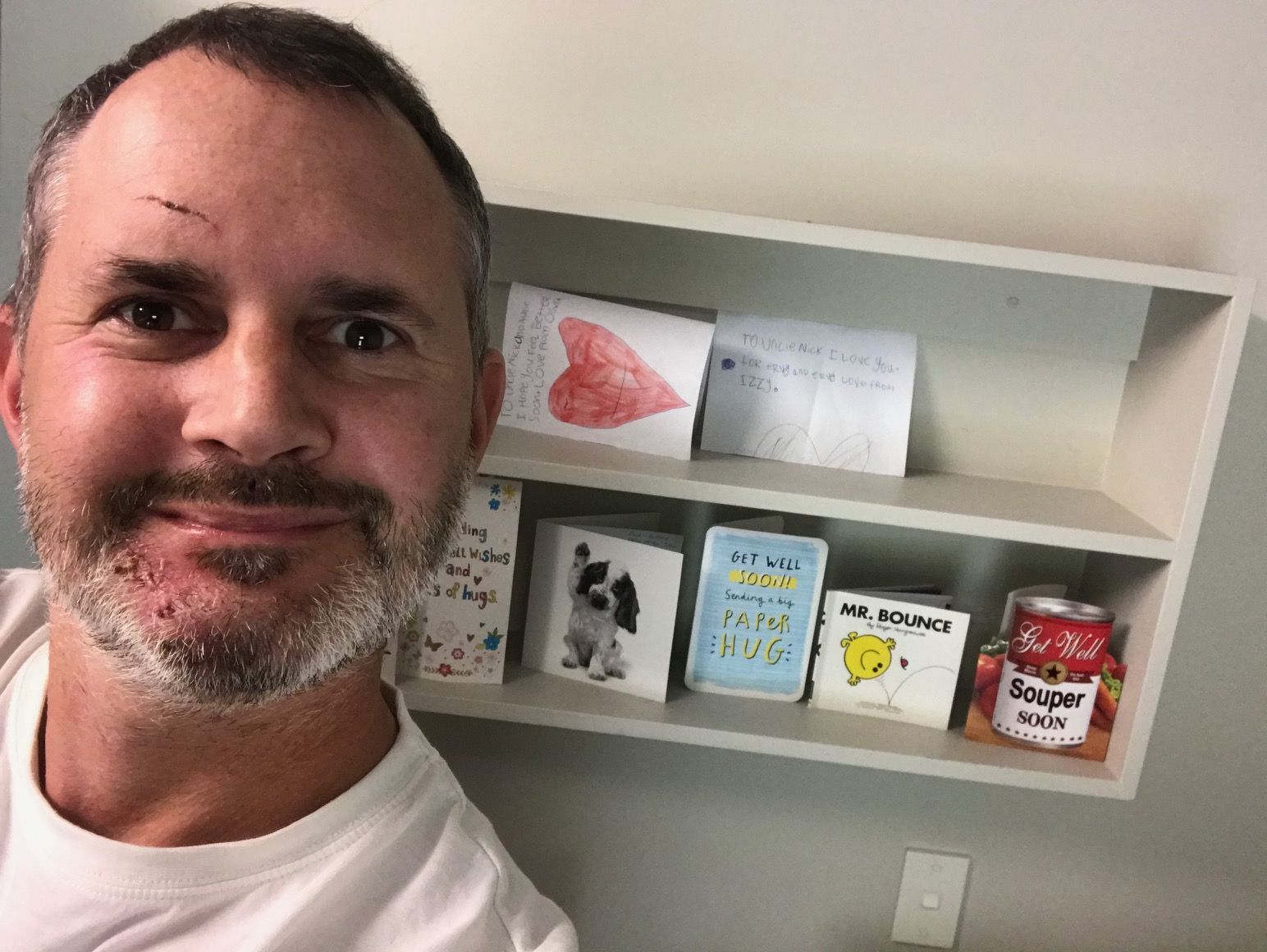
I can remember more about the visitors I had here – check ins, catch ups and just general chats with the friends, colleagues and family that came to see how I was getting on – seeing those visitors just made my day every time without fail – it was so nice to connect with people.

More fatigue was always around the corner. A constant reminder I was actually recovering & due for a rest. Don’t push it Nick. It’s a journey.
My activities got more advanced – challenges, daily living tasks such as making myself lunch, balancing & walking – slowly, I was allowed to watch some more TV & use my iPad or iPhone. Slowly things were getting better. Except the fatigue, still present, but now I’d had some advice on what to look out for & how to manage that side of things.
I felt more comfortable in the unit as the days went on – safe, secure, genuinely cared for, which I am very thankful for. The staff were very understanding when I didn’t get things quite right, was a bit jumbled or said the wrong word (another work on) – to me I felt I was treated like a normal person, with some friendly help along the way. It was great to be able to start making decisions for myself like when I’d head out for a walk or get some exercise or when I needed to get some rest – it was all thanks to the support I had from my carers & I’m grateful I had the experts there to help me.
My new lifestyle
As I mentioned earlier usually I was an active, all systems go type person who didn’t take well to sitting back & watching the days go by. The new lifestyle that I found myself temporarily fitting in with at times led to feelings of frustration & boredom which gave me new challenges to face – mainly adjusting to how things had to be for my own good. It wasn’t easy but the main thing I had to focus on was the wise words, guidance & advice I was receiving which in a nutshell spelled out that slowing down & taking my time was good for myself in the long run. I guess the trump card I had in all of this was a positive mindset that helped adopt everything so I could adjust to the new ‘normal’.
I still remember being somewhat nervous when my partner & I met with a ‘panel’ (not really, it just felt like one) of the Laura Fergusson team to discuss & review my progress to date as well as the next steps. Before the meeting I remember being a bit anxious & thinking “Do I appear to have fully recovered? Can I go home? Are they going say I have to stay in the unit longer?”, but it was really my overactive imagination thinking the worst so you can imagine how great it was to get the feedback & news that I’d made progress & I was closer to being able to head home.
First I would have a ‘trial run’ being at home over a weekend. I had a few tasks to complete such as a daily log of how I felt, a schedule to follow but most of all was the excitement of being able to get back to my own home, give my partner a hug at night, see my cat and all the normal day to day things I was craving that we generally take for granted that I hadn’t been part of for a while.
As well as the usual fatigue, one of my work-on's was related to my (now pretty below average) memory and the unfamiliarity of previous experiences – things that were common to me sometimes seemed new so I had a good set of guidelines to follow; nothing too strenuous – a short trip each day, maybe a quiet walk; aim to stick to a daily structure – lunch & dinner at the usual times; get up/go to bed at the same time each day & no late nights; be smart - if you’re tired, have a rest or a nap during the day. Pretty basic stuff, but important for me to follow & stick to.
I liked being at home but in a way, it didn’t feel familiar either – I almost felt like I was a guest at someone’s house. Old sights or things felt new again, as it seemed like I was experiencing them for the first time. On reflection as we’d been away at Christmas before my accident it was over a month since I’d been at home so I hadn’t been there for a good while.
It was a bit of a confusing feeling as I’d been so keen to get home & hadn’t obviously realised the positive impact that being in the Laura Fergusson unit had made on me & provided me during my recovery at that time. The benefit was that I clearly felt comfortable, safe & competent in the unit, more so that my own house, so I think is a good thumbs up for how important that step was & the support plus assistance that the staff gave me.
On the Monday morning I went back to the Laura Fergusson unit & felt kind of glad to be back in a familiar place with friendly faces. I picked up where I left off, continuing my normal recovery pathway interacting with the various specialist staff & debriefed with them how my weekend went. I stayed my last night as an “in-patient” & then I was given the all clear to head home for good on the Tuesday. By this time it felt right to be going home & I was looking forward to it, feeling more comfortable as well as having learnt that I was a bit more confident in my ability to manage on my own so to speak.
One of the questions I had before I was discharged was about which organisation I was going to nominate to assist in supporting my rehabilitation next steps from home. I had all the various options explained to me, but I opted to remain under the care of the Laura Fergusson team – it gave me continuity of care and it had been a positive experience so far. One of the bonuses was that quite a few of the same people I was familiar with were going to continue supporting me.
My big aim at home was to make a conscious effort to stick to all the strategies & routines I’d been used to in the rehabilitation unit as I was getting some small wins & I figured I’d be silly not to adhere to the advice I’d been given.
My specialist appointments were ongoing plus I also had an assigned ACC Case Worker who was a great resource to help with arranging things to make life just a bit easier like a taxi allowance. I enjoyed having the specialists visit me at my home in among the daily challenges I was giving myself & the ongoing visits to the hospital & my GP to sort out my other physical injuries which were still on the mend.
It was a slow & steady process this recovery thing. I know my approach was a crucial win for me; I was conscious to be aware of my limits & applied the learning I’d had to date. I listened to all the advice & strategies that my team were telling me & was applying them. I soaked up the constructive feedback as well as enjoyed the positive feedback I received. Even if they were small wins I stayed positive. Sure, I had bad days & it wasn’t always plain sailing but it was like they say in the clichés; a journey – it won’t be quick & you can’t rush things, it won’t always be as expected, but you’ll get there.
I could see I was on the right track & it was so reassuring to often be told I was ahead of where I ‘should be’ at this stage of my recovery. Each time I heard that it really made me remember how far I had come – often that was just what I needed to keep working on me.
I liked the experts being a troubleshooting resource for me & I could talk to them about any concerns, issues or questions that I had; I was never made to feel like I had a silly or simple question. I quickly learnt too that the more open & honest I was about how I felt & how I was doing meant the better outcomes I was getting. I had real trust in my team of people.
Getting to know my new limits & accepting them as the new normal was something that couldn’t be rushed, but things became easier to accept as time went on & I was able to process it all & come to terms with it. I knew that some things just weren’t happening right now like driving a car, being able to ride a bike or get back & do my part at work. At the start I’ll admit I would get a bit frustrated about receiving medical certificates with extended dates in advance or the information I received about when I might be able to drive again but it was because I was determined to get things back on track & was often willing things to come right sooner than I knew they probably would.
Looking back
Looking back I think that I was able to accept & come to terms with it all because even though they were sometimes small, I could notice & feel the improvements happening – whether it was mundane things like a doing a basic everyday task we’d normally do without a thought, I came to realise that it was all part of the healing process & that while often not perfect or frustrating, it was just going to take time. The thing is as everyone kept telling me, no one can tell you exactly how & when your recovery will go – the time frames of where you’ll be in 3/6/12 months are the experts best assumptions based on what they know – it’s not a one size fits all recovery plan & every patient responds & recovers differently.
I also learnt I didn’t always know or wasn’t aware of what my capabilities were at a certain time. You might think you’re doing OK & not even think about it too much – I learnt this quickly when my Physio visited one day & tested my balance. It was so shocking I couldn’t believe how bad it was, but some quick reassurance from her put me at ease that like some other aspects it would come right & was actually a common thing & was just another work on. The flipside was sometimes I thought I wasn’t doing so well at all with something but when I was ‘tested’ or assessed I learnt I was actually doing OK.
As time went on I was more & more keen to reconnect & be involved with the ‘normal’ real world – do hobbies, tick off jobs, do stuff with friends & get back to work all best I could, the quicker the better. I was lucky that the Laura Fergusson team really saw I was ready for the next step & that I was on the right track to dip my toes back into my work.
My Occupational Therapist had some honest meetings with my Manager & I to make sure we were all on the same page about how things might work for me making a return to work which involved a very gradual re-integration plan. To this day I still feel very fortunate to have such an understanding & supportive employer, Manager & team of people that I work with because it has made a real difference for me & a big impact on my recovery to date. I’ve never felt pressured by work, my Laura Fergusson team or by ACC to get back to 100% - actually quite the opposite at times, as its usually me wanting to take on too much too soon, so I have a great group of people helping to keep me in check & make sure I take things easy.
I remember the first day I stepped back into the office – part excitement, part nervousness, part fear – but safe to say I had nothing to be concerned about as I was looked after so well as I started out doing 2 hours a day, for 3 days a week. You might think that sounds like a walk in the park but let me tell you it’s OK to be totally stuffed after that kind of effort, so much so that you have a nap on the couch in the afternoon at home!
I’ve since increased my hours each week from that start & now am working a good few hours each day. I still catch up with all my support crew at Laura Fergusson & look forward to each session.
So, like I mentioned earlier it’s a journey, it takes time. There are ups & there are downs but it does get easier, & over time things slowly continue to get back to normal.
My best advice like I said that worked for me is to accept the new normal & take the advice that you’re given. Don’t be hard on yourself & accept the small wins.